This post is a part of a series called “Help Me Understand,” where we practice the art of dialogue amongst diverse opinions. The focus is to come around the table and learn to have healthy conversations with people whose views are different from our own.
In January, my friend *Lucy wrote to me, “I’m so sorry for my delay. Over the last few days, we attended a friend’s funeral and were helping her family with childcare.”
Lucy’s friend died in childbirth, leaving behind a husband, a newborn and oceans of unexpected grief.
My heart ached with fear and sadness. My great-grandmother died in childbirth in the 1940s. My grandfather lived his entire life with inescapable grief. Even though I knew this deep pain and had read the statistics about maternal mortality in the United States, it still seemed unfathomable that a healthy woman could die in childbirth in New York City in 2020.
Recently, Sha-Asia Washington, a 26-year-old Black woman from Brooklyn, died following an emergency cesarean section. Her story shed light again on the pervasive racial disparities Black women face in the health care system. The United States has the highest maternal mortality rate among developed countries. Among, American women, Black women are the most vulnerable.
In order to advocate for change, we must first understand the contributing factors to maternal death, including our fractured healthcare system and its underlying systemic racism.
The Risk American Women Face
Between 700 and 900 American women die annually in the maternal period. Death can occur during pregnancy, in childbirth or within 42 days following birth. Experts estimate that at least two-thirds of these deaths could be prevented. While other developed nations are seeing a decline in maternal mortality rates, in America, maternal mortality rates are worsening. Between 1991 and 2014, maternal mortality rates doubled from 10.3 to 23.8 deaths per 100,000 live births.
American mothers are at least three times more likely to die compared to Canadian mothers. They are also six times as likely to die compared to Scandinavian mothers.
A Fractured Healthcare System
A study comparing maternal outcomes of 11 high-income countries (including Canada, Sweden and the United Kingdom) found that American mothers were at a higher risk of pregnancy complications due to higher rates of chronic illness, higher rates of C-sections, less access to quality healthcare and higher costs for medical services.
Postpartum care for American mothers is severely lacking. Though more than 50% of maternal deaths happen postpartum, new mothers in the U.S. often only attend one follow-up appointment for themselves four to six weeks after giving birth. In other countries, where the public health systems are more robust, midwives and nurses visit women several times at home in the postpartum period.
Measuring the Problem
The U.S. differs from other nations in how it counts and deals with maternal deaths—a key factor in understanding maternal mortality. ProPublica reports that maternal deaths are treated as “private tragedies” rather than as failures of the American medical system. Families deal with their confusion, outrage and grief privately without clear answers.
Until recently, “pregnancy” was not an option on death certificates, making it nearly impossible to accurately measure maternal mortality in the U.S. This contrasts starkly with the U.K. where the government widely publishes national maternal health data. There is also a standing committee of experts that scrutinizes all evidence in each maternal mortality case, and medical examiners hold public inquiries that require hospitals to explain each failure.
The Most at Risk Demographic: Black Women
While all American women face a higher risk of maternal mortality than other nations, the burden falls on Black American women, who are 243% more likely to die from childbirth or pregnancy. According to the Center for Disease Control and Prevention, in the U.S., Black mothers die at three to four times the rate of white mothers, one of the widest of all racial disparities in women’s health.
In New York City, Black mothers are 12 times more likely to die in the maternal period. Studies have shown that educational achievement and socioeconomic wealth did not improve outcomes for Black women. In New York, highly educated and wealthy Black mothers are still significantly more at risk for complications and death than uneducated white mothers.
Race impacts nearly every aspect of maternal medicine. Black women experience higher rates of toxic stress (due to systemic racism) and are, therefore, more at risk for chronic illnesses and more likely to give birth through C-sections. Yet, they are treated with a lower standard of care.
Black women’s symptoms and pain are often not taken seriously or acted upon urgently. For example, when Serena Williams gave birth in 2017, she knew she was at greater risk in childbirth because of her history with blood clots and pulmonary embolisms. Following her C-section, she nearly died from manifold complications.
Racism within maternal healthcare creates dangerous ripple effects. Black women who have been discriminated against by their medical team are less likely to attend follow-up postpartum appointments for themselves, even when they keep prenatal and pediatrician appointments for their newborns.
Historical Racism in the American Medical System
There is a long history of racial bias within American medicine which underscores the failures of the healthcare system. Called the “father of modern gynecology,” James Marion Sims performed experimental surgery on enslaved women, children and infants without anesthesia. In the Tuskegee Study, hundreds of Black men were not treated for syphilis, even after penicillin was discovered as a cure. Instead, they were observed by researchers as they suffered and died.
A biopsy of Henrietta Lacks’ cancer cells were used to create the first “immortal cell line” without her family’s consent. Throughout the 20th century, state-sponsored programs sterilized thousands of women of color without their knowledge or consent.
This pattern of dehumanization shapes current medical treatment. Researchers have documented how doctors underprescribed opioid painkillers to Black patients. While this may have prevented opioid addiction in Black communities, this racial bias (tied to the racist myth that Black people do not experience or experience less pain) left Black patients suffering without treatment.
Today, only 4% of physicians and 7% of medical school graduates are Black. When Black patients are treated by Black doctors, they receive more preventative services, and the doctor-patient relationship usually benefits from an increased sense of safety, mutual trust and open communication. Improving representation in the medical field may improve maternal outcomes as well.
The realities of maternal mortality in the United States are frightening for women, especially Black women. Not all hope is lost, though. Groundswell community efforts, like the Birthing Project USA, support expectant mothers of color throughout every stage of pregnancy with incredible results. States like California have employed strategies to make pregnancy and birth safer, bringing maternal mortality rates down to be on par with outcomes in U.K. and Portugal.
As we envision new possibilities for the American healthcare system, we must push for a federal system that addresses the racial disparities that threaten Black mother’s lives. We need a healthcare system built on anti-racist principles that offered complete and compassionate care to all American women.
*The name has been changed to Lucy to protect her privacy.
Why do you think Black women are more likely to face pregnancy-related complications and face a higher risk of mortality in American medicine? What can you do to advocate for them?
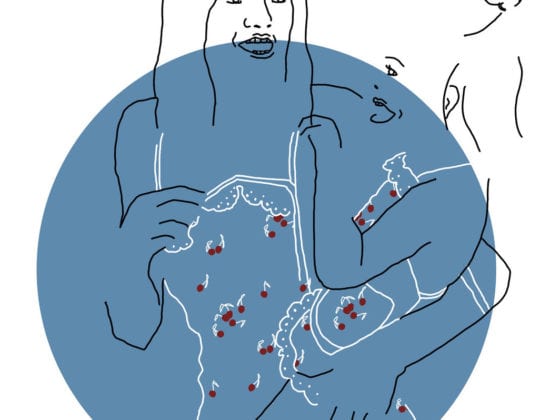
Image via Kat Borchart, Darling Issue No. 15